Clostridium difficile infection, diarrhea and probiotics
- Video
- 5 min
What is Clostridium difficile?
Clostridium difficle is a harmful bacteria that is often responsible for major hospital outbreaks of diarrhea.1 C. difficile infections make up approximately 12% of all hospital infections.2
What are the symptoms of a C. difficile infection?
C. difficile infections can be very serious, and are found in up to 30% of patients who are experiencing antibiotic-associated diarrhea.1
One of the problems linked with C. difficile infections is that people can have recurrent infections. In fact, 20% of people who have a C. difficile infection for the first time will have a recurrent infection, and 60% of people who have already relapsed.1
The most common symptom is diarrhea, however if the disease becomes severe, there can be other symptoms.3
Mild to moderate disease:
- Diarrhea with other symptoms not consistent with severe or complicated disease3
Severe disease:
- Diarrhea3
- Either increased white blood cell numbers or abdominal tenderness3
Complicated:
- Admission to intensive care3
- Low blood pressure3
- Fever3
- Swollen abdomen3
- Increased white blood cell numbers3
- Increase in serum lactate levels 3
- Failure of organs such as kidneys3
- Change in mental status such as confusion3
Serious complications from C. difficile infection can lead to death.4
What are the causes of C. difficile disease?
C. difficile can survive for months in conditions that do not favour its growth, such as outside the human body.1 This is one of the reasons that it can be transmitted so easily. 1 Many of the people who have C. difficile are asymptomatic and do not know that they have the bacteria, therefore they can spread it further.2
Risk factors for developing a C. difficile infection include : 1,3
- Antibiotic treatment
- Age >65 years
- Hospitalisation
- Surgery
- Poor hygiene
- Chemotherapy or cancer
- Proton pump inhibitors
- Inflammatory bowel diseases
- Immunosuppression
How does C. difficile cause diarrhea?
C. difficile infections cause diarrhea when they produce harmful toxins.1 In fact, many people have non-harmful, non-toxin producing C. difficile as part of their microbiota.1
These toxins cause diarrhea by : 5
- Activating inflammation which results in the increase of water into the intestine
- Destroying intestinal cells and stopping the cells from being in contact with each other.
How do we treat C. difficile infections?
Untreated, C. difficile infections can lead to much more serious conditions including colitis (chronic digestive disease).1 As it is quickly spread, with many people carrying the bacteria but not showing symptoms, addressing these infections is very important.2
The first step is to prevent transmission, which means correct infection control procedures such as handwashing and disinfection to prevent the spread.2
As C. difficile overgrowth in the gut is associated with antibiotic treatment, treating with antibiotics can alter the gut microbiota further.6 This may create an environment that further supports the growth of C. difficile.6 This means that unnecessary antibiotic treatment will be avoided, and normally, one of two antibiotics will be prescribed (metronidazole or vancomycin).2 For recurrent C. difficile infection that is resistant to antibiotic therapy, patients can receive a fecal microbiota transplant.3
It has been reported that preventing an initial C. difficile infection is the most effective way to address C. difficile.2
Preventing the disruption to the microbiota that can arise with antibiotic use can be one way to prevent C. difficile infection.7 One way to prevent the disruption to the microbiota is to use probiotics.7
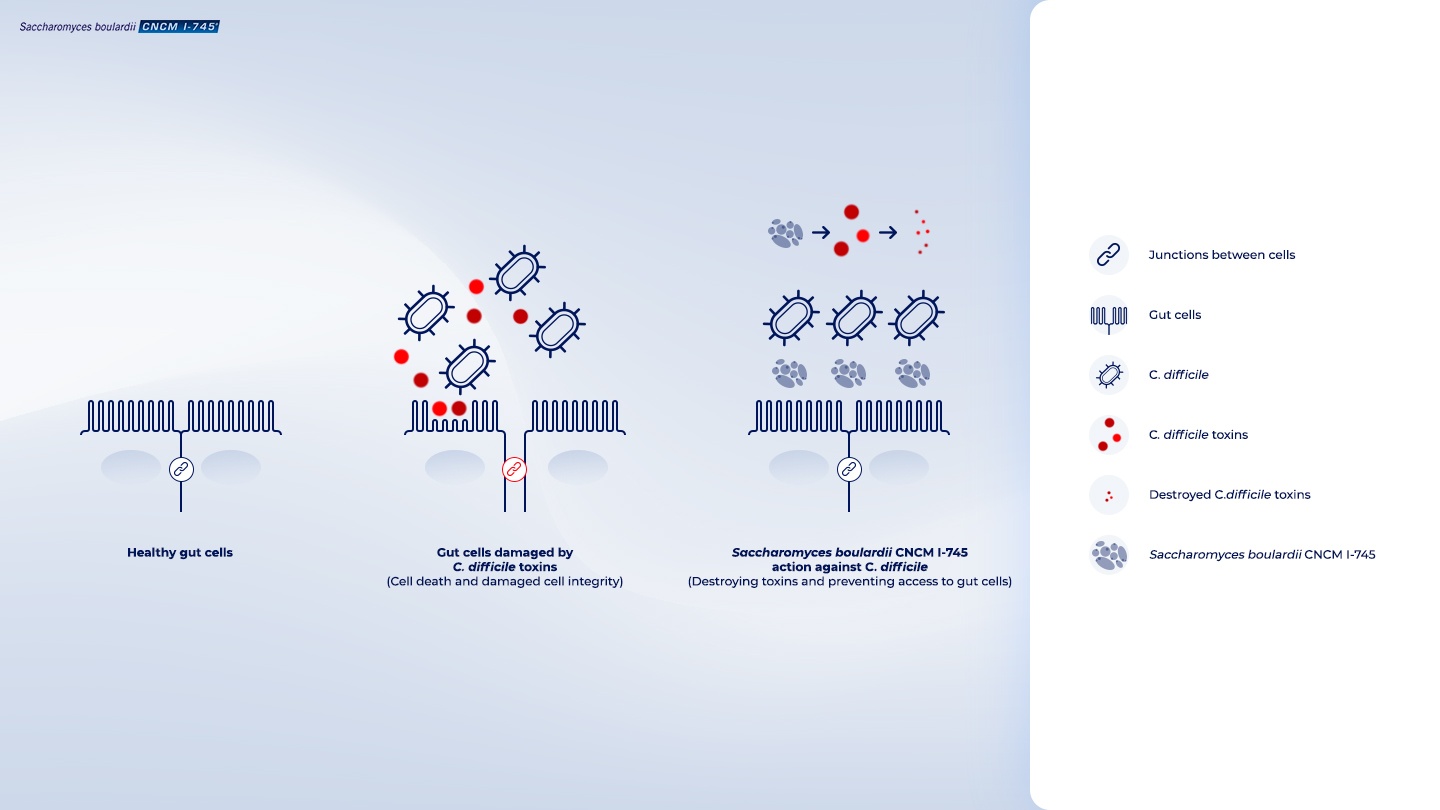
The probiotic Saccharomyces boulardii CNCM I-745 prevents C. difficile infections during antibiotic treatment
Studies have shown that taking the single-strain yeast probiotic Saccharomyces boulardii CNCM I-745 during or following antibiotic treatment reduces the risk of both primary and recurrent C. difficile infections.6,7-9
In addition to the recommended antibiotic therapy for C. difficile infection, taking this specific yeast probiotic strain reduces the risk of recurrent infection between 57%6 and 66%9.
S. boulardii CNCM I-745 effectively prevents this infection during antibiotic treatment by : 1
- Targeting the C. difficile toxins and destroying them
- Stopping C. difficile from binding to the gut cells
(Internal code : 20.60)
Furthermore, it helps maintain and restore the normal microbiota diversity in the gut by creating the right environment. This promotes the growth of beneficial microbes and restores the balance in the gut, which also helps reduce the occurrence of diarrhea.10
Therefore, Saccharomyces boulardii CNCM I-745 not only prevents C. difficile infections during antibiotic treatment, helps create a healthy gut environment after the infection.6-10
Internal code : 20.11
References
- 01 . Joly, F et al. 2017. Saccharomyces boulardii CNCM I-745. Marteau, P and Dore J (Ed.), Gut Microbiota: A full-fledged organ. 2017: 305-326. Paris: John Libbey Eurotext. Gut Microbiota Book.
- 02 . McFarland, LV. Primary prevention of Clostridium difficile infections – how difficult can it be? Expert Review of Gastroenterology & Hepatology. 2017. DOI: 10.1080/17474124.2017.1312343.
- 03 . Surawicz CM, et al. Guidelines for diagnosis, treatment, and prevention of Clostridium difficile infections. The American journal of gastroenterology. 2013; 108(4): 478.
- 04 . Sunenshine RH, and McDonald, CL. Clostridium difficile-associated disease: new challenges from an established pathogen. Cleveland Clinic journal of medicine. 2006; 73(2): 187.
- 05 . Di Bella, Stefano, et al. Clostridium difficile toxins A and B: insights into pathogenic properties and extraintestinal effects. Toxins. 2016; 8(5): 134.
- 06 . McFarland LV, et al. A randomized placebo-controlled trial of Saccharomyces boulardii in combination with standard antibiotics for Clostridium difficile disease. Jama. 1994; 271(24): 1913-1918.
- 07 . Kotowska M, et al. Saccharomyces boulardii in the prevention of antibiotic-associated diarrhea in children: a randomized, double-blind placebo-controlled trial. Alimentary pharmacology & therapeutics. 2005; 21(5): 583-590.
- 08 . McFarland, LV. Probiotics for the primary and secondary prevention of C. difficile infections: a meta-analysis and systematic review. Antibiotics. 2015; 4(2): 160-178.
- 09 . Surawicz, CM, et al. The search for a better treatment for recurrent Clostridium difficile disease: use of high-dose vancomycin combined with Saccharomyces boulardii. Clinical infectious diseases. 2000; 31(4): 1012-1017.
- 10 . More MI, and Swidsinski, A. Saccharomyces boulardii CNCM I-745 supports regeneration of the intestinal microbiota after diarrheic dysbiosis–a review. Clinical and experimental gastroenterology. 2015; 8: 237.
