Taking probiotics has multiple positive effects on the gut and its microbiota
- Video
- 7 min
What are probiotics?
Probiotics are living microorganisms that, when taken in adequate amounts, offer a health benefit to the host.1 Probiotics that are most commonly used can be either bacterial or yeast microbes.1
Why are probiotics beneficial?
The benefit of probiotics in gut functioning is related to their influence on the gut microbiota.1
Microbiota are trillions of microorganisms that live in a mutually beneficial relationship with the gut.1 These microorganisms are found mainly in the colon, and offer many benefits including stimulation of immune function and fermentation of substrates that contribute to the host cell nutrition.2
The gut microbiota is introduced from birth, mainly from the mother and also from the environment.2 The microbiota that is present after birth changes during the first three years of life and reaches a “stable” population in the adult years.3 However, during those first years, the microbiota population that is established is influenced by factors including gestational age, mode of birth delivery, breastmilk vs bottle-fed, exposure to antibiotics or short-term illnesses.2 Disturbances to diversity of microbiota in those early years can lead to allergies and obesity later in life.3
In adults, the gut microbiota diversity and composition can be affected by many factors including diet, exposure to medications (e.g. antibiotics), illness and age.3 The results can include diarrhea, inflammatory conditions and overgrowth of harmful bacteria.4
Probiotics work by positively affecting the ecosystem of the gut.1 They do this by either creating an environment that favours the growth and re-establishment of normal gut microbiota, improving gut physiology (including increasing the mucus barrier which prevents harmful bacteria from accessing cells), digest food, or influencing the immune system (including increasing the secretion of antibodies that can target harmful bacteria).1,3
How to choose a probiotic?
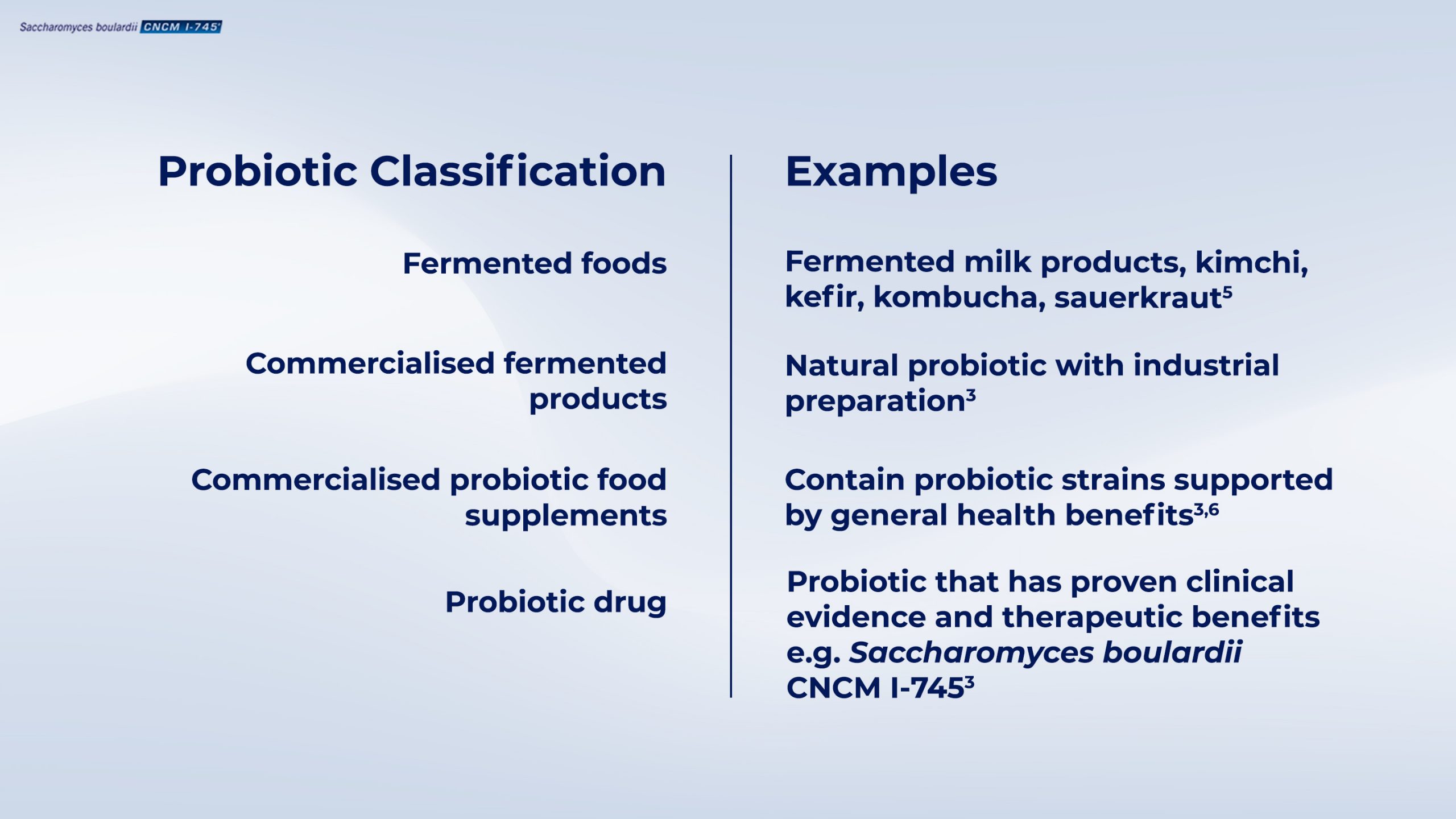
Probiotics exist in different forms3, such as fermented foods, supplements, and probiotic drugs3 (Table 1).
(Internal code : 20.60)
A probiotic should not be confused with a prebiotic, which is a fermentable ingredient (usually non-digestible carbohydrates) that is a food source for microbiota and probiotics.1 For example, breast milk and sugars found in certain fruits such as bananas are prebiotics.1 Nor should it be confused with postbiotics, products or metabolites produced by bacteria that also offer health benefits, but are not living organisms.7
The classification of a probiotic as a drug, food or food supplement also reflects the level of clinical evidence regarding efficacy and safety.3 A probiotic food or food supplement does not exert therapeutic action, but may have health benefits.3 A probiotic food is consumed in a balanced diet while a probiotic food supplement is aimed to supplement a normal diet.3
A probiotic label may not describe all the strains it contains.9 This is very important as some probiotics offer different health benefits compared to others, and not all strains have the same level of clinical evidence that demonstrates their health benefit.3,8
Also, probiotics can be manufactured differently, require different storage conditions and contain different numbers of strains.1 Some probiotics can be affected by antibiotics10, while some may not survive the harsh conditions of the stomach3 and therefore there are less reaching the gut.1 For example, a bacterial species commonly found in fermented dairy products (Lactococcus lactis) has high sensitivity to acid and bile and only lasts for a short time in the gut.11
Why is Saccharomyces boulardii CNCM I-745 a good choice of probiotic?
Saccharomyces boulardii CNCM I-745 is a unique single-strain yeast probiotic. It is the first discovered probiotic drug and offers multiple gastrointestinal benefits.3 S. boulardii CNCM I-745 has many advantages that make it suitable as a probiotic, such as:
- Naturally non-susceptible to antibiotics so it can be taken at the same time as antibiotics10 ;
- Can tolerate acidic nature of stomach which means that it can survive and pass through to the intestine4 ;
- Grows at human body temperature (37°C) unlike other yeast probiotics4 ;
- Does not permanently colonize the gut, which means that the normal balance of microbiota is not disturbed by its presence.4
Due to its long history, S. boulardii CNCM I-745 has strong clinical evidence demonstrating its efficacy including :
- Stimulating immune responses to prevent colonization by harmful bacteria that can lead to a disruption of the normal gut microbiota diversity.4
- Acting on harmful bacterial species such as Clostridium difficile to prevent overgrowth or prevent the activity of toxins3 ;
- Treating acute diarrhea associated with infection1 ;
- Restoring the normal microbiota diversity following a disruption such as antibiotic treatment4 ;
Because of the strong clinical evidence,
Internal code : 20.57
References
- 01 . Guarner et al. Probiotics and prebiotics. World Gastroenterology Organisation Global Guidelines. February 2017. https://www.worldgastroenterology.org/guidelines/global-guidelines/probiotics-and-prebiotics/probiotics-and-prebiotics-english. Last accessed 14th November 2019.
- 02 . Butel, MJ, Waligora-Dupriet AJ, and Wydau-Dematteis, S. The developing gut microbiota and its consequences for health. Journal of developmental origins of health and disease. 2018; 9(6): 590-597.
- 03 . Joly, F et al. Gut Microbiota: A full-fledged organ. 2017. Marteau, P and Dore J (Ed.). Paris: John Libbey Eurotext.
- 04 . More MI, and Swidsinski, A. Saccharomyces boulardii CNCM I-745 supports regeneration of the intestinal microbiota after diarrheic dysbiosis–a review. Clinical and experimental gastroenterology. 2015; 8: 237.
- 05 . Terefe, N. Food Fermentation. Reference Module in Food Science. Elsevier. 2016. ISBN 9780081005965. Pages 1-3. https://doi.org/10.1016/B978-0-08-100596-5.03420-X.
- 06 . De Simone, Claudio. The unregulated probiotic market. Clinical Gastroenterology and Hepatology. 2019; 17(5): 809-817.
- 07 . Aguilar-Toalá JE, et al. Postbiotics: An evolving term within the functional foods field. Trends in Food Science & Technology. 2018; 75: 105-114.
- 08 . Kolacek S, et al. Commercial probiotic products: A call for improved quality control. A Position Paper by the ESPGHAN Working Group for Probiotics and Prebiotics. Journal of pediatric gastroenterology and nutrition. 2017; 65(1): 117-124.
- 09 . Recommendations of AGA. https://www.gastro.org/practice-guidance/gi-patient-center/topic/probiotics/choosing-the-right-probiotics. Last accessed 20th January 2020.
- 10 . Neut C, Mahieux S, and Dubreuil LJ. Antibiotic susceptibility of probiotic strains: is it reasonable to combine probiotics with antibiotics? Medecine et maladies infectieuses. 2017; 47(7): 477-483.
- 11 . Marteau P, Shanahan F. Basic aspects and pharmacology of probiotics: an overview of pharmacokinetics, mechanisms of action and side-effects. Best Pract Res Clin Gastroenterol 2003 ;17 : 725-740.
- 12 . Cruchet et al. The Use of Probiotics in Pediatric Gastroenterology: A Review of the Literature and Recommendations by Latin-American Experts. Pediatric Drugs. 2015; 17:199-216.
- 13 . Szajewska H, et al. Probiotics for the prevention of antibiotic-associated diarrhea in children. Journal of Pediatric Gastroenterology and Nutrition. 2016; 62(3): 495-506.
- 14 . Malfertheiner P, et al. Management of Helicobacter pylori infection—the Maastricht V/Florence consensus report. Gut. 2017; 66(1): 6-30.
- 15 . Cameron D, et al. Probiotics for gastrointestinal disorders: proposed recommendations for children of the Asia-Pacific region. World journal of gastroenterology. 2017; 23(45): 7952.
- 16 . Ghoshal UC, et al. The role of the microbiome and the use of probiotics in gastrointestinal disorders in adults in the Asia‐Pacific region‐background and recommendations of a regional consensus meeting. Journal of gastroenterology and Hepatology. 2018; 33(1): 57-69.
- 17 . Guarino A, et al. European Society for Pediatric Gastroenterology, Hepatology, and Nutrition/European Society for Pediatric Infectious Diseases evidence-based guidelines for the management of acute gastroenteritis in children in Europe: update 2014. Journal of pediatric gastroenterology and nutrition. 2014; 59(1): 132-152.
