Antibiotic-associated diarrhea: the unexpected consequence of taking antibiotics
- Video
- 4 min
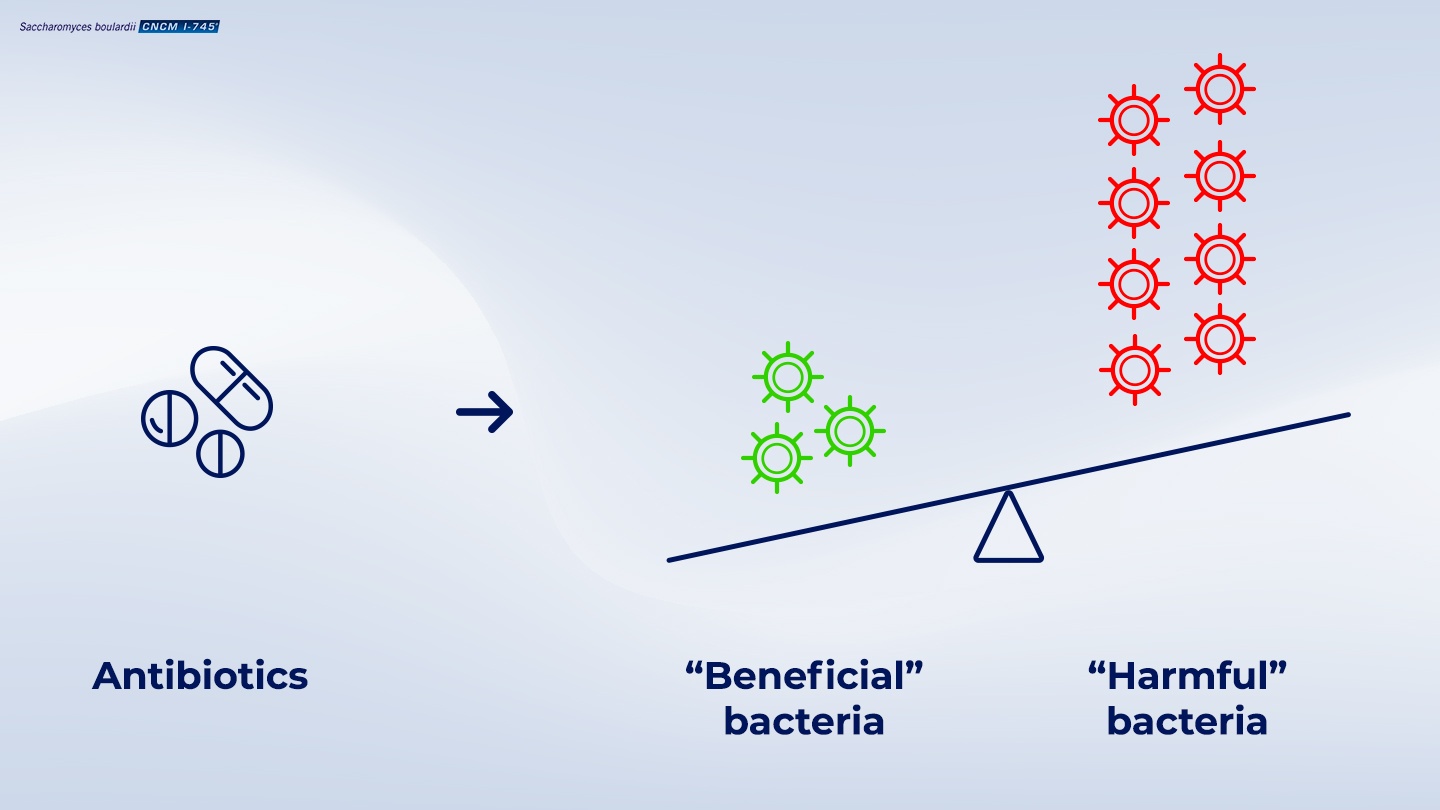
Taking antibiotics has a negative impact on microbiota and gut health
The gut microbiota, a collection of microbes that reside in the gut, influence many physiological processes, from immune system regulation to metabolism.1 These microbes consist mostly of bacteria.2 This means that the gut microbiota can be affected by antibiotic treatment.1
While antibiotics are an important treatment approach for many infectious diseases,
The change in microbiota diversity caused by taking antibiotics means that the natural balance of beneficial and harmful bacteria in the intestinal tract is altered.2,3 The change in microbiota diversity often results in increased numbers of harmful bacteria.3
(Internal code : 20.60)
The harmful bacteria compete with the normal microbiota for nutrients and can produce substances that destroy the beneficial bacteria, as well as create toxins that affect the normal gut function.4
The change in microbiota is generally a short-term consequence of taking antibiotics, however,
What are the consequences of taking antibiotics?
The major consequence of antibiotic-induced changes to gut microbiota diversity is antibiotic-associated diarrhea (AAD).1 Diarrhea is the signal that there is an imbalance in the diversity of the microbiota in the gut.1 AAD generally occurs during antibiotic treatment, however diarrhea can occur 2 to 8 weeks after treatment has finished.4
How quickly AAD occurs can be influenced by the type of antibiotic and the type of harmful bacteria that increases in the gut following antibiotics can influence the severity/rate at which AAD develops.4 For example, 1/3 of AAD cases are caused by the bacteria Clostridium difficile4, and is often recurrent.4
Health consequences associated with antibiotics :
Short-term effects associated with antibiotics4
- Experience of diarrhea (loose, watery stools for >2 days; early onset occurring during antibiotic treatment, or delayed onset occurring 2-8 weeks after antibiotic treatment)
Long-term consequences associated with antibiotics4
- C. difficile infection
- Recurrent antibiotic-associated diarrhea
- Increased risk of antibiotic resistance
- Complications such as colitis (an inflammation of the colon) or pseudomembranous colitis are the more serious complications associated with antibiotic therapy.
Who is at risk of developing antibiotic-associated diarrhea?
Up to 35% of adults receiving antibiotics experience antibiotic-associated diarrhea (AAD).4 However, AAD occurs in a wide variety of populations including outpatients and residents of long-term care facilities4, with risk-associated factors such as a history of AAD, young or elderly age4 and co-morbidities.4
Factors associated with an increased risk of developing antibiotic-associated diarrhea : 3,4
- History of AAD
- Age (elderly, young)
- Continuous tube-feeding
- Antibiotics: oral administration; broad spectrum (cephalosporin, penicillin); biliary elimination; continuous antibiotic therapy; multiple antibiotics use
Saccharomyces boulardii CNCM I-745 is an effective approach to prevent, treat and recover from antibiotic-associated diarrhea.
Probiotics are living microorganisms that when administered in adequate amounts confer a health benefit.6 The single-strain yeast probiotic Saccharomyces boulardii CNCM I-745 is proven to help reduce the occurrence of antibiotic-associated diarrhea.6 For example, it has been demonstrated that the occurrence of diarrhea is reduced by 53% in adults when Saccharomyces boulardii CNCM I-745 is taken at the same time as antibiotics.6 In addition the yeast reduces the impact of antibiotics on the microbiota during treatment.7
Unlike bacterial probiotics, S. boulardii CNCM I-745 is naturally resistant to antibiotics which means that it can be taken at the same time as antibiotics to act on the immediate effect of the antibiotics on the microbiota and reduce the risk of antibiotic-associated diarrhea.8
Internal code : 20.07
References
- 01 . Francino, MP. Antibiotics and the human gut microbiome: dysbioses and accumulation of resistances. Frontiers in microbiology. 2016; 6: 1543.
- 02 . Panda S, et al. Short-term effect of antibiotics on human gut microbiota. PloS one. 2014; 9(4): e95476
- 03 . McFarland, LV. Epidemiology, risk factors and treatments for antibiotic-associated diarrhea. Digestive Diseases. 1998; 16(5): 292-307.
- 04 . McFarland LV. Antibiotic-associated diarrhea: epidemiology, trends and treatment. Future Microbiology. 2008; 3(5): 563-578.
- 05 . Palleja A, et al. Recovery of gut microbiota of healthy adults following antibiotic exposure. Nature microbiology. 2018; 3(11): 1255.
- 06 . Szajewska H, and Kolodziej, M. Systemic review with meta-analysis: Saccharomyces boulardii in the prevention of antibiotic-associated diarrhea. Alimentary pharmacology & therapeutics. 2015; 42(7): 793-801.
- 07 . Kabbani TA, et al. Prospective randomized controlled study on the effects of Saccharomyces boulardii CNCM I-745 and amoxicillin-clavulanate or the combination on the gut microbiota of healthy volunteers. Gut microbes. 2017; 8(1): 17-32.
- 08 . Neut C, Mahieux S, and Dubreuil LJ. Antibiotic susceptibility of probiotic strains: is it reasonable to combine probiotics with antibiotics?. Medecine et maladies infectieuses. 2017; 47(7): 477-483.
